
About Rectal Prolapse
Copyright 2009-2014 Saviz Inc. All rights reserved.
What is Rectal Prolapse?
Rectal prolapse is a condition in which the rectum (the lower end of the colon, located just above the anus) turns itself inside out. In the earliest phases of this condition, the rectum does not stick out of the body, but as the condition worsens, it may protrude. Weakness of the anal sphincter muscle is often associated with rectal prolapse at this stage and may result in leakage of stool or mucus. The condition occurs in both sexes, although it is more common in women than men.
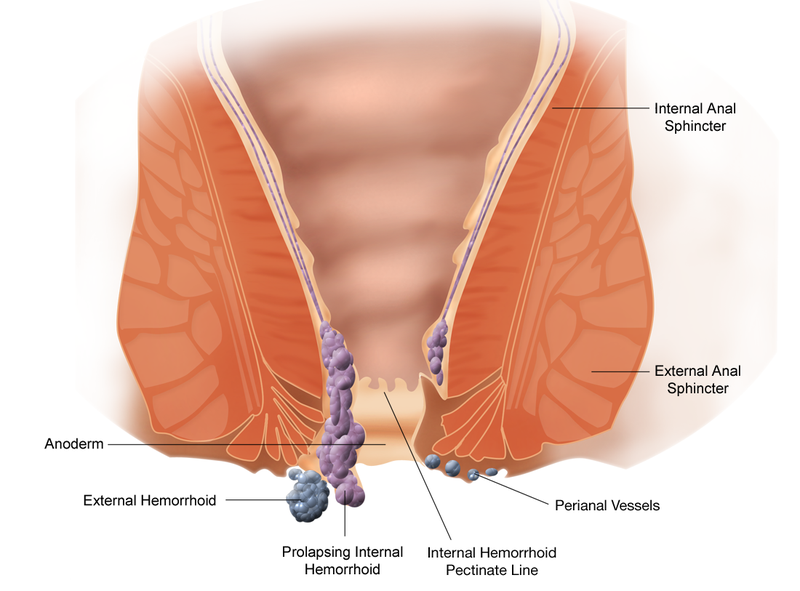
Is Rectal Prolapse the same as hemorrhoids?
Some of the symptoms may be the same. There may be bleeding and/or tissue that protrude from the rectum. Rectal prolapse, however, involves a segment of the bowel located higher up within the body, while hemorrhoids develop near the anal opening.
How is Rectal Prolapse treated?
Although constipation and straining may be causes of rectal prolapse, simply correcting these problems may not improve the prolapse once it has developed. There are many different ways to surgically correct rectal prolapse.
Abdominal or rectal surgery may be suggested. Your doctor can help you decide which method will most likely achieve the best result by taking into account many factors, such as age, physical condition, extent of prolapse and the results of various tests.
Treatment of rectal prolapse depends on several factors:
- Patient's age
- Physical condition
- Extent of prolapse
- Test results
Why does it occur?
Several factors may contribute to the development of rectal prolapse. It may come from a lifelong habit of straining to have bowel movement or as a delayed result of stresses involved in childbirth. In rare cases, there may be a genetic predisposition in some families. It seems to be a part of the aging process in many patients who experience weakening of the ligaments that support the rectum inside the pelvis as well as loss of tightness of the anal sphincter muscle. In some cases, neurological problems, such as spinal cord transaction or spinal cord disease, can lead to prolapse. In most cases, however, no signal cause can be identified.
How is Rectal Prolapse diagnosed?
Your physician can diagnose this condition by taking a careful history and performing a complete anorectal examination. To demonstrate the prolapse, patients may be asked to "strain" as if having a bowel movement or to sit on the commode and "strain" prior to examination.
At times, however, a rectal prolapse may be "hidden" or interval. In this situation, an X-ray examination called a videodefecogram may be helpful. This examination, which takes X-ray pictures while the patient is having a bowel movement, can also assist the physician in determining whether surgery may be beneficial and which operation may be appropriate.
Anorectal manometry may also be used. This test measures whether or not the muscles around the rectum are functioning normally.
How successful is treatment?
Success depends on a number of factors, including the status of a Patient's anal sphincter muscle before surgery, whether the prolape is internal or external, the overall condition of the patient and surgical method used. If the anal muscle has been weakened, either because of the rectal prolapse or for some other reason, it may in many cases significantly regain strength after the rectal prolapse has been corrected.
Chronic constipation and straining after surgical correction must be avoided. A great majority of patients are completely relieved of symptoms, or are significantly helped, by the appropriate procedure.

.jpg)





.jpg)
