
Colon (anatomy)
The colon is the last part of the digestive system in most vertebrates; it extracts water and salt from solid wastes before they are eliminated from the body, and is the site in which flora-aided (largely bacterial) fermentation of unabsorbed material occurs. Unlike the small intestine, the colon does not play a major role in absorption of foods and nutrients. However, the colon does absorb water, sodium and some fat soluble vitamins.
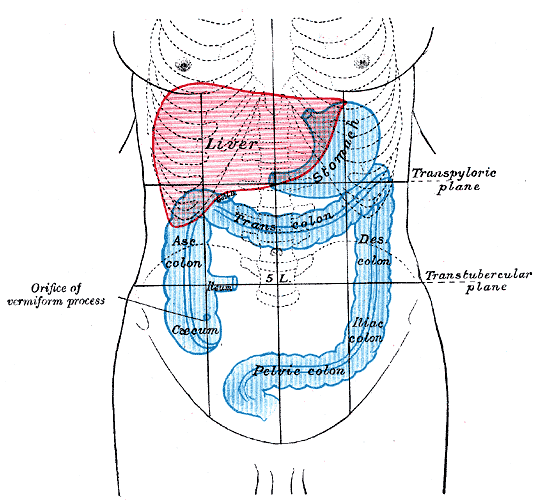
In mammals, the colon consists of four sections:
The ascending colon,
The transverse colon,
The descending colon,
The sigmoid colon (the proximal colon usually refers to the ascending colon and transverse colon).
The colon, cecum, and rectum make up the large intestine.
The location of the parts of the colon is either in the abdominal cavity or behind it in the retroperitoneum. The colon in those areas is fixed in location.
The haustra of the colon are the small pouches caused by sacculation, which give the colon its segmented appearance. The taenia coli runs the length of the large intestine. Because the taenia coli is shorter than the intestine, the colon becomes sacculated between the taenia, forming the haustra.
Anatomy
The ascending colon, on the right side of the abdomen, is about 13 cm long in humans. It is the part of the colon from the cecum to the hepatic flexure (the turn of the colon by the liver). It is secondarily retroperitoneal in most humans. In ruminant grazing animals, the cecum empties into the spiral colon.
Anteriorly it is related to the coils of small intestine, the right edge of the greater omentum, and the anterior abdominal wall. Posteriorly, it is related to the iliacus, the iliolumbar ligament, the quadratus lumborum, the transverse abdominis, the diaphragm at the tip of the last rib; the lateral cutaneous, ilioinguinal, and iliohypogastric nerves; the iliac branches of the iliolumbar vessels, the fourth lumbar artery, and the right kidney.
The ascending colon is supplied by parasympathetic fibers of the vagus nerve (CN X).
Arterial supply of the ascending colon comes from the ileocolic artery and right colic artery, both branches of the SMA. While the ileocolic artery is almost always present, the right colic may be absent in 5–15% of individuals.
Ascending colon
Blood supply and lymphatics
Arterial supply to the colon comes from branches of the superior mesenteric artery (SMA) and inferior mesenteric artery (IMA). Flow between these two systems communicates via a "marginal artery" that runs parallel to the colon for its entire length. Historically, it has been believed that the arc of Riolan, or the meandering mesenteric artery (of Moskowitz), is a variable vessel connecting the proximal SMA to the proximal IMA that can be extremely important if either vessel is occluded. However, recent studies conducted with improved imaging technology have questioned the actual existence of this vessel, with some experts calling for the abolition of the terms from future medical literature.
Venous drainage usually mirrors colonic arterial supply, with the inferior mesenteric vein draining into the splenic vein, and the superior mesenteric vein joining the splenic vein to form the hepatic portal vein that then enters the liver.
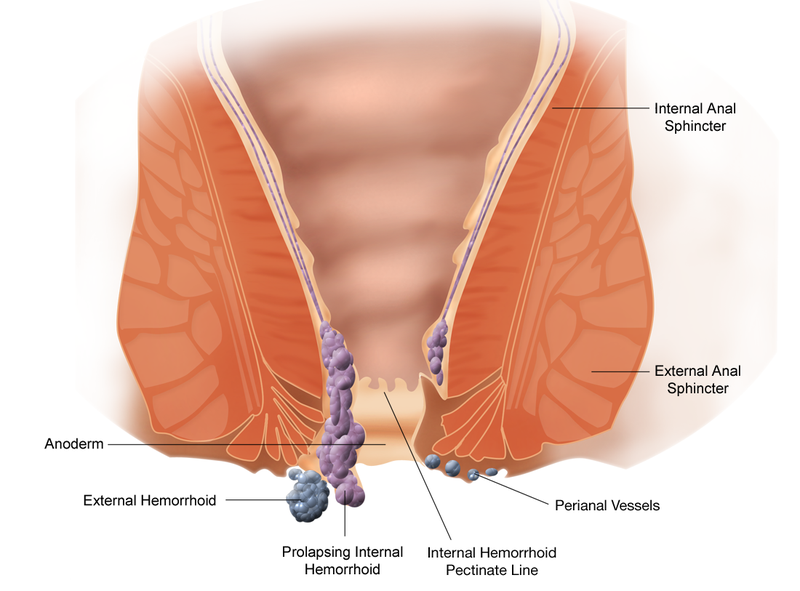
Lymphatic drainage from the entire colon and proximal two-thirds of the rectum is to the paraaortic lymph nodes that then drain into the cisterna chyli. The lymph from the remaining rectum and anus can either follow the same route, or drain to the internal iliac and superficial inguinal nodes. The pectinate line only roughly marks this transition
The transverse colon is the part of the colon from the hepatic flexure to the splenic flexure (the turn of the colon by the spleen). The transverse colon hangs off the stomach, attached to it by a wide band of tissue called the greater omentum. On the posterior side, the transverse colon is connected to the posterior abdominal wall by a mesentery known as the transverse mesocolon.
The transverse colon is encased in peritoneum, and is therefore mobile (unlike the parts of the colon immediately before and after it). Cancers form more frequently further along the large intestine as the contents become more solid (water is removed) in order to form feces.
The proximal two-thirds of the transverse colon is perfused by the middle colic artery, a branch of SMA, while the latter third is supplied by branches of the IMA. The "watershed" area between these two blood supplies, which represents the embryologic division between the midgut and hindgut, is an area sensitive to ischemia.
Transverse colon
The descending colon is the part of the colon from the splenic flexure to the beginning of the sigmoid colon. The function of the descending colon in the digestive system is to store food that will be emptied into the rectum. It is retroperitoneal in two-thirds of humans. In the other third, it has a (usually short) mesentery. The arterial supply comes via the left colic artery.
Descending colon
The sigmoid colon is the part of the large intestine after the descending colon and before the rectum. The name sigmoid means S-shaped (see sigmoid). The walls of the sigmoid colon are muscular, and contract to increase the pressure inside the colon, causing the stool to move into the rectum.
The sigmoid colon is supplied with blood from several branches (usually between 2 and 6) of the sigmoid arteries, a branch of the IMA. The IMA terminates as the superior rectal artery.
Sigmoidoscopy is a common diagnostic technique used to examine the sigmoid colon.
Sigmoid colon
One variation on the normal anatomy of the colon occurs when extra loops form, resulting in a longer than normal organ. This condition, referred to as redundant colon, typically has no direct major health consequences, though rarely volvulus occurs resulting in obstruction and requiring immediate medical attention.[4] A significant indirect health consequence is that use of a standard adult colonoscope is difficult and in some cases impossible when a redundant colon is present, though specialized variants on the instrument (including the pediatric variant) are useful in overcoming this problem.
Redundant colon
Water absorption at the colon typically proceeds against a transmucosal osmotic pressure gradient. The standing gradient osmosis is a term used to describe the reabsorption of water against the osmotic gradient in the intestines. This hypertonic fluid creates an osmotic pressure that drives water into the lateral intercellular
spaces by osmosis via tight junctions and adjacent cells, which then in turn moves across the basement membrane and into the capillaries.
Standing gradient osmosis
What's Colon & Rectum?
Copyright 2009-2014 Saviz Inc. All rights reserved.
.png)
.jpg)
.jpg)





.jpg)